BHRS: Living with COVID - Challenges and Benefits of Changes
Published: 14 May 2020
-
Views:
 1109
1109
-
Likes:
 7
7
-
Views:
 1109
1109
-
Likes:
 7
7
-
 2m 50sPart 1 Introduction: Living with COVID Francisco Leyva, Mauro Biffi
2m 50sPart 1 Introduction: Living with COVID Francisco Leyva, Mauro Biffi
-
 16m 48sPart 2 Continuing Cardiology: During and after COVID Howard Marshall
16m 48sPart 2 Continuing Cardiology: During and after COVID Howard Marshall
-
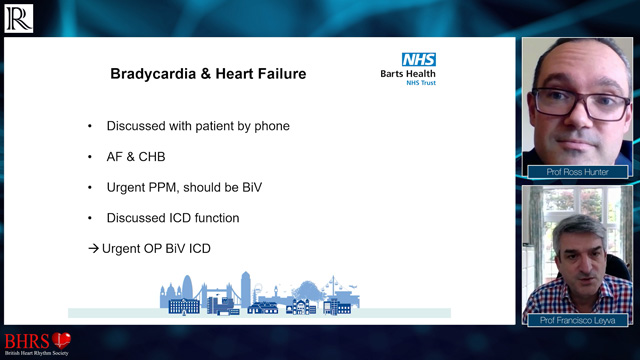
 20m 15sPart 3 Remote Clinics & Investigations: What Have We Learnt During COVID? Ross Hunter
20m 15sPart 3 Remote Clinics & Investigations: What Have We Learnt During COVID? Ross Hunter
-
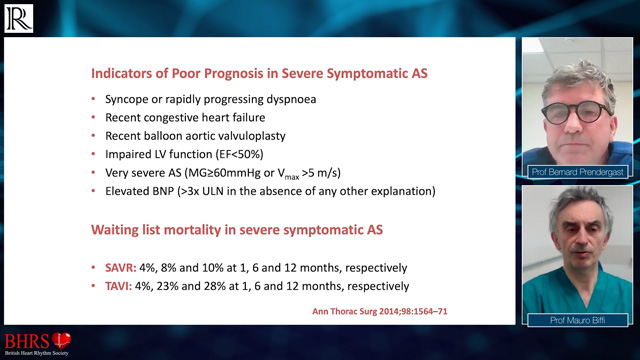
 14m 18sPart 4 BNP and ECG as a Guide to Picking up Significant Valvular Heart Disease Bernard Prendergast
14m 18sPart 4 BNP and ECG as a Guide to Picking up Significant Valvular Heart Disease Bernard Prendergast
-
 17m 19sPart 5 Imaging in the Era of COVID: Who Needs Imaging When Resources Are Limited? Nik Sabharwal
17m 19sPart 5 Imaging in the Era of COVID: Who Needs Imaging When Resources Are Limited? Nik Sabharwal
Overview
Prof Francisco Leyva and Prof Mauro Biffi introduce this online video series, filmed in partnership with the BHRS. Through a series of 8 videos, they explain how faculty aim to draw parallels on hospital responses during the COVID-19 crisis and assess how treating patients in cardiology has been during this period and how cardiologists will continue to operate in what will be the new ‘normal’.

More from this programme
Part 1
Introduction: Living with COVID
| 1 session | |
| Introduction: Living with COVID | Watch now |
Part 2
Continuing Cardiology: During and after COVID
Part 3
Remote Clinics & Investigations: What Have We Learnt During COVID?
Part 4
BNP and ECG as a Guide to Picking up Significant Valvular Heart Disease
Part 5
Imaging in the Era of COVID: Who Needs Imaging When Resources Are Limited??
Part 6
Running a Remote Device Clinic with Cases during and after COVID-19
Part 7
Opportunities and Challenges with Remote Services during and after COVID-19
Part 8
Patient Satisfaction With Remote Services During and After COVID-19
Part 9
Closing Remarks: Living with COVID
| 1 session | |
| Closing Remarks: Living with COVID | Watch now |
Faculty Biographies

Matt Swift
Cardiac Physiologist
Matthew Swift is the lead Cardiac Physiologist for CRM at the Great Western Hospital, Swindon. His professional interests include the optimisation of CRT devices, programming ICDs and improving the patient experience while increasing patient safety.














